Name: Ian Emmerson
Age: 69
Diagnosis: COPD, pneumonia, heart failure
When Ian Emmerson was rushed to hospital with breathing problems last winter, he felt exhausted and confused.
Although he hadn’t been feeling well, the 69-year-old had thought the breakdown of a recent relationship was to blame and that all he needed was a good night’s sleep.
In fact, Ian had suffered a heart attack. After undergoing tests, he was sent home to recover.
Within less than a week, Ian was back in hospital with pneumonia. And a week later, he was hospitalised once again with the lung condition, chronic obstructive pulmonary disease (COPD).
“It was frightening because I was very ill but had to keep going home, where I was alone. It was hard to simply look after myself,” he says.
Sadly, his story is not unique. This winter, the NHS hit the headlines after a surge in demand from patients in accident and emergency departments.
Like Ian, many were older and suffering from long-term health problems that they could not keep on top of at home.
While it isn’t good for the overall health of patients like Ian to constantly be rushed to A&E, it is also bad for the wider NHS. More patients put more pressure on hospital beds and more strain on limited NHS budgets.
According to NHS England’s Forward Plan published last year, the way these patients are cared for needs to change fundamentally.
“The NHS needs to adapt to take advantage of the opportunities that science and technology offer patients, carers and those who serve them,” the plan says.
MSD is passionate about developing and providing service solutions to the NHS that meet customers’ needs so they can deliver the best care and outcomes possible for patients
It says that improving the care of these patients within the community is key. But it’s not just the NHS which needs to help achieve this. Health industries who work with the NHS must also change.
Merck Sharp and Dohme (MSD) has spent decades developing important new medicines and vaccines. Although this will always remain its foundation, it has now set up its Healthcare Services division to tackle the much more pressing question of how to improve patient care.
Michael Nally, vice president and managing director, MSD UK, says: “MSD is passionate about developing and providing service solutions to the NHS that meet customers’ needs so they can deliver the best care and outcomes possible for patients. As a true healthcare company, we use our in-depth knowledge and expertise in the healthcare sector to develop and provide a diverse portfolio of service offerings.”
Using its passion for research and evidence-based medicine, MSD Healthcare Services aims to improve patient care and reduce healthcare costs, but in a way that is independent of their pharmaceutical and vaccine division.
Closercare, for example, had patients like Ian in mind. This patient monitoring service allows patients with long-term conditions, such as heart failure and COPD, to have their health monitored remotely while staying in the comfort of their own home.
[embed_related]
The idea is simple: patients are given a bag containing, for example, weighing scales, a blood pressure monitor, an oximeter (depending on their condition) and a smartphone.
Every day, they carry out basic health checks and the devices send the results wirelessly through to their smartphone, which also records how they feel that day, and sends them on to a team of Closercare nurses.
If the patient’s results are abnormal, it triggers a red flag to the nurses who ring the patient and either monitor them more closely or contact their local community nursing team, or other relevant clinician on behalf of the patient.
Ian was offered Closercare just after he returned home from his third stay in hospital. “As I’m on my own, it was good to know that someone was caring and keeping an eye on me,” he says. “I’d send through my results every day and if there was a problem they’d always ring. They were very polite and I cannot speak highly enough of them to be honest. It’s been a brilliant service during my recovery.”
MSD Healthcare Services has worked hard to make sure that all their products are evidence based.
Another problem for GPs can be identifying patients with long-term conditions who have the greatest clinical need.
MSD Informatics is software that has already been adopted by one in five practices in the UK since its inception in 1998. The software allows health professionals to spot patients with complex health problems who might not be hitting treatment targets – whether Quality Outcomes Framework targets or local targets – as well as gaps in their prescriptions.
For some NHS regions, problems may lie around a particular disease area. MSD’s Evidence into Practice is an award-winning programme that creates bespoke data, workshops and expert input for individual practices on how to improve care.
In NHS Greenwich, Evidence into Practice was used to improve diabetes care after it emerged that performance across the region could be improved.
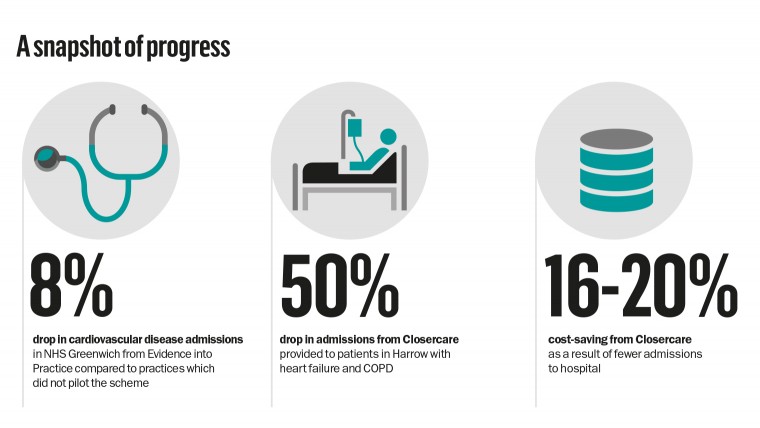
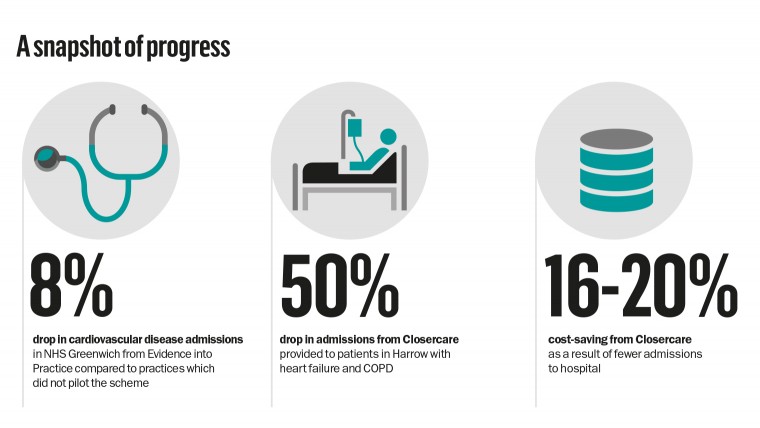
Practices saw a 12 per cent drop in outpatient diabetic medicine attendances and 8 per cent drop in cardiovascular disease admissions compared to increases in both these among practices which did not pilot the scheme. It also saved more than £70,000 per 100,000 population.
The NHS Forward Plan says: “A better future is possible – and with the right changes, right partnerships and right investments, we know how to get there.”
Ian is one patient who shows how this can be done. “I’m almost back to what I was,” he says. “I’m on lots of tablets, but at least I’m here. We’re getting there.”
TAKING A CLOSER LOOK
In Harrow Clinical Commissioning Group, Closercare was provided to patients with heart failure and COPD last year. Over three months, there was a 50 per cent drop in admissions, a 12 per cent reduction on A&E attendances and 66 per cent drop in bed days. Some of this may be due to other changes in treatment, but much is due to the patient monitoring service. It also achieved a 16-20 per cent cost-saving as a result of fewer admissions to hospital.
David Barrett, a lecturer in nursing from the University of Hull, who independently evaluated the trial, says: “If you can spot patients who are getting ill early on, you can treat them quickly and avoid a sudden admission to hospital. Telehealth – remote patient monitoring – makes people feel reassured that someone is keeping an eye on them and taking their own blood pressure or weighing themselves each day may also help them to take more responsibility for their own health. Telehealth can be extremely useful in a number of ways.”
This commercial feature was developed and supported by MSD Healthcare Services