Coronary heart disease is not something many of us expect to suffer with. So for the two million people in the UK who have the condition, diagnosis can come as a huge shock.
Figures from the Office for National Statistics show it is now the leading single cause of avoidable death in Britain.
The burden of this condition on both patients and their families is huge. Patients often need medication as well as surgery to unblock the blood vessel and many doctors will recommend patients have a stent inserted.
But experts believe the most complicated cases should be offered a cardiovascular operation known as a coronary bypass graft or CABG instead. In the UK, around 20,000 patients a year have this type of surgery.
David Taggart, professor of cardiovascular surgery at the University of Oxford, says CABG is a good option for patients.
 “There is overwhelming evidence that for most patients, CABG gives a better long-term outcome in terms of survival as well as a reduced risk of further heart attacks and the need for any more stents,” he says. “But even though there is already overwhelming evidence for CABG, we should still ask the question, ‘Could the results be even better?’”
“There is overwhelming evidence that for most patients, CABG gives a better long-term outcome in terms of survival as well as a reduced risk of further heart attacks and the need for any more stents,” he says. “But even though there is already overwhelming evidence for CABG, we should still ask the question, ‘Could the results be even better?’”
Although CABG can provide astonishing results in patients with severe coronary heart disease, estimates suggest that between 5 and 11 per cent of grafts will fail. Often this is because surgeons are not aware the new graft they have just created does not work properly.
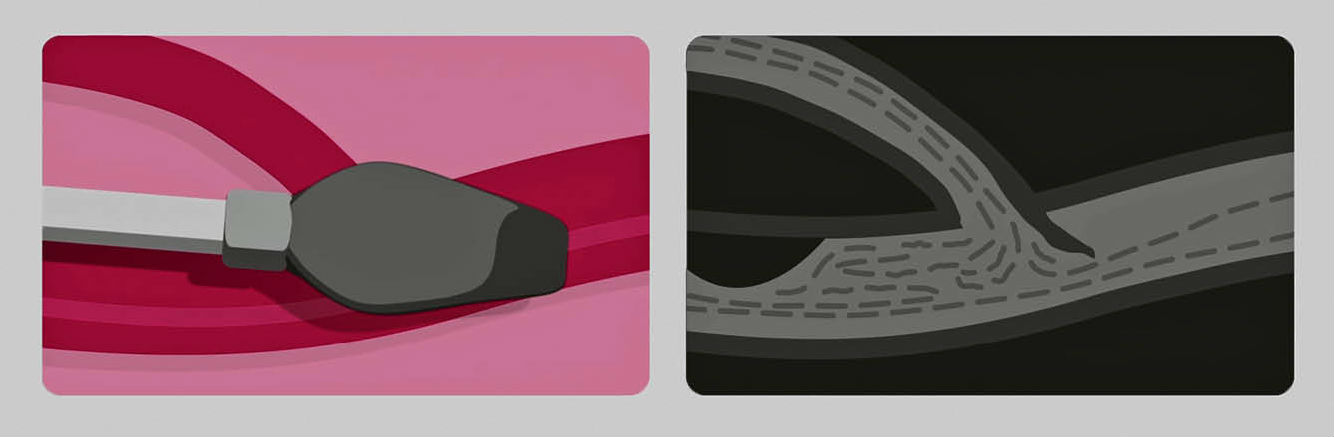
Coronary artery bypass grafts use a section of a blood vessel taken from another part of the body such as the chest or leg. This is stitched to the coronary artery to create a bypass around a blockage, allowing blood to flow freely to the heart.
Key to the success of the operation is checking to see if blood is flowing properly through the graft before the patient leaves the operating room. The case for measuring blood flow during CABG is compelling.
A 2010 Canadian study by Kieser et al showed that measuring graft function using TTFM (transit time flow measurement) during the operation gave surgeons a score that indicated how well the surgery had gone. Grafts that scored above a five tended to leave patients at higher risk of a serious adverse event later. The study showed that major cardiac events occurred in 17 per cent of patients who scored highly compared with 5.4 per cent of patients with a lower score.

Transit time flow measurement (TTFM) is used to verify graft function
Following non-emergency surgery, 9 per cent of patients with the higher reading died compared with only 2 per cent who had the lower reading.
Using a scoring system during surgery was therefore pivotal to helping surgeons understand if they needed to make revisions to the grafts while the patient was still on the operating table.
According to guidance issued to NHS doctors in 2011 by the National Institute for Health and Clinical Excellence (NICE), a tool developed by Norwegian firm Medistim was shown to reduce the risk of graft failure and risk of morbidity and mortality linked to the operation for patients, while still saving the NHS money.
“Hospital teams may want to use the VeriQ system because it can reduce problems after coronary artery bypass graft surgery that are caused by graft failure and may reduce the length of time people need to stay in hospital,” the NICE guidance states.
Despite this, most NHS hospitals have still not adopted use of the technology during CABG surgery. Currently, fewer than one in twenty operations in the UK assess the graft using the technology.
The advantage of this device is that it allows the surgeon to prove they really have done a great job
This compares starkly to Japan where more than 80 per cent of surgeons use TTFM and Germany where around 70 per cent of surgeons have adopted it.
Medistim has funded Professor Taggart to carry out research using their device on patients in Oxford.
“The advantage of this device is that it allows the surgeon to prove they really have done a great job,” he says. “In my research, we have found that about one in twenty bypass grafts have a problem that could be resolved while the patient is still in the operating room if the surgeon knew.
“But often the surgeon will not know that there is a problem until after the operation when complications can arise in either blood pressure or an abnormal ECG. In fact it may not become obvious until after the patient has left the hospital.
“It is well established that for one specific type of CABG graft, the mammary artery, it actually increases life expectancy. So it is intuitive to check that this graft really is patent before the patient leaves the operating room.
“The surgeon must be certain because the implications for the patient are so great. If it was me or my family having this operation, I would do my best to make sure the surgeon had checked the patency of the grafts before I left the operating room.”
Medistim has more than 30 years’ experience in making medical devices and their latest to come to market, the MiraQ system, is unique. The technology combines two types of probes to be used during cardiac surgery from the same system.
An ultrasonic imaging probe enables surgeons to decide where they should place the graft. The image allows them to detect and avoid areas of the aorta that are calcified or lined with soft plaques. This information is critical because dislodging the plaques can cause them to travel straight to the brain, triggering a stroke.
The second flow-measuring probe can then check that blood flow through the new graft is acting normally. The device sends ultrasound beams across the blood vessel and the return signal is analysed and displayed on a touch screen. Resulting data shows blood flow through the vessel in millilitres per minute and provides readings that indicate if the graft has been successful.
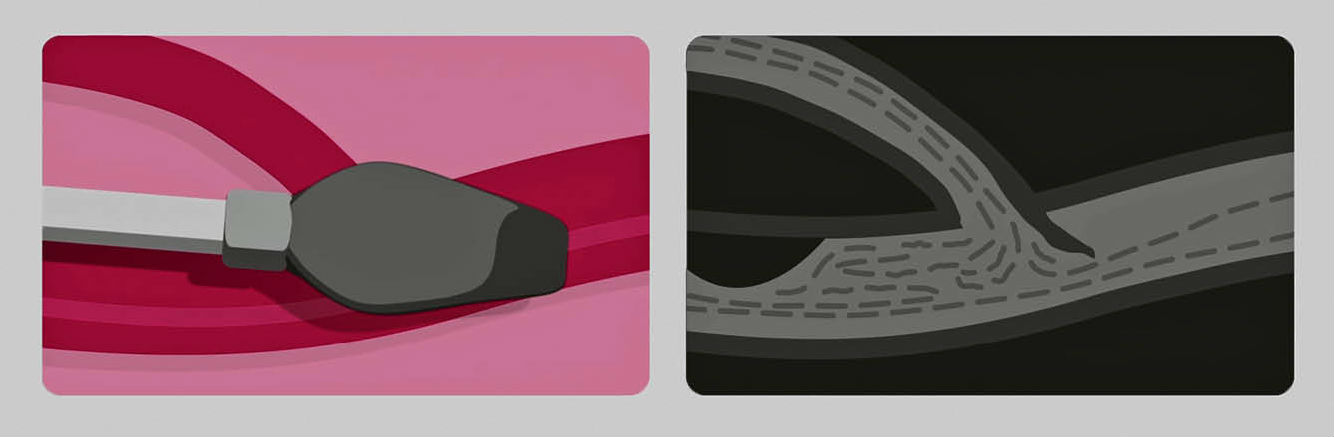
Ultrasound imaging provides information from the inside of the vessel to check for possible obstructions of the blood flow
Professor Heinz Jakob, director of the Department of Cardiothoracic Surgery at the West German Heart Centre in Essen, has used TTFM for almost two decades.
“This device creates a safety net for surgeons and it saves the lives of patients. It is a really important tool for our staff, especially when training young cardiac surgeons in indicating low bypass flow in case of anastomotic mistakes, thus helping to prevent infarction,” he says.
“The new imaging device enables us quickly to find hidden coronary arteries in re-do situations and adds visualisation of anastomoses to pure flow measurement, an additional step forward for safety. Surely it is in the interest of surgeons to get the best result possible for their patients?”
For more information please visit medistim.com