Spring is here and longer days are upon us. As we shed our winter layers and spend more time outdoors, many of us seek this opportunity to top up our vitamin D levels, having been starved of sunshine in the greyer months.
However, there remains a strong, resounding message from the dermatology community that we should all be wearing regular sunscreen to protect against skin cancer.
To see the full infographic click here
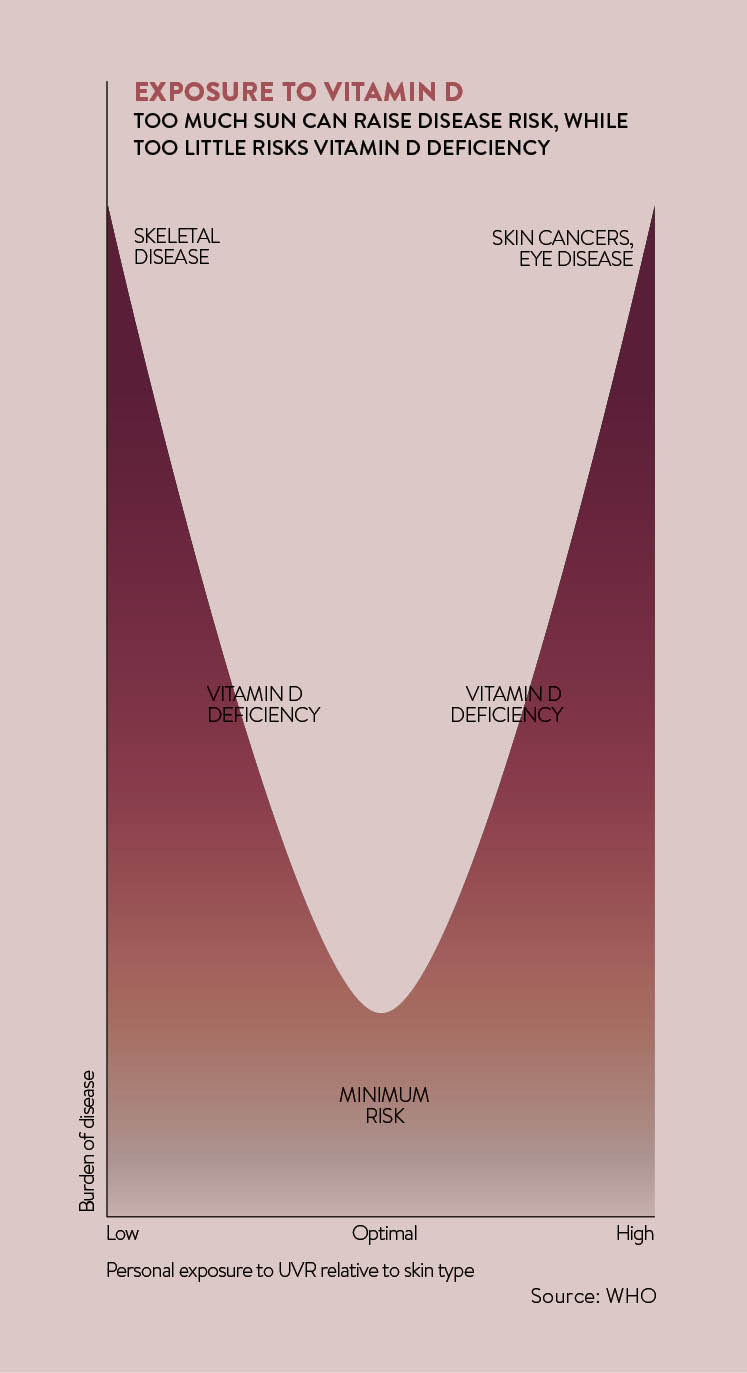
Often, the messages can be confusing. On the one hand, we clearly need vitamin D from sunshine to maintain health; on the other, no one knowingly wants to be put at risk of developing cancer.
We clearly need vitamin D from sunshine to maintain health, but no one knowingly wants to be put at risk of developing cancer
So how do we go about balancing the risks? What should we be doing to look after both our skin and our general health?
The benefits of Vitamin D
Vitamin D is a fat-soluble vitamin essential for maintaining bone health. Shahir Hamdulay, consultant physician and rheumatologist at The Wellington Hospital in London, explains: “Deficiency of vitamin D is highly prevalent worldwide and attributed in part to inadequate sunlight exposure.” Deficiency will lead to weakening of the bones, resulting in rickets in children and osteomalacia or osteoporosis in adults.
There is also evidence to suggest vitamin D provides protection against some types of cancer, heart disease, multiple sclerosis and diabetes, as well as providing benefits to mood and wellbeing. Dr Hamdulay adds: “These important roles need to be considered when protecting the skin.”
An individual’s vitamin D status can be checked with a simple blood test to measure serum 25-hydroxyvitamin D levels. Authorities generally agree that laboratory levels below 25nmol/L are deficient.
Unprotected sun exposure is the major source of vitamin D production for most adults and children in the UK. Sunlight, in particular ultraviolet-B (UVB) radiation, drives vitamin D synthesis in skin. The amount of UVB radiation to which we are exposed depends on the time of day, season and latitude. In the UK it is highest between the hours of 10am and 3pm at the height of summer. Vitamin D production also varies from person to person, with dark or pigmented skin requiring longer UVB exposure to synthesise equivalent amounts.
[embed_related]
The British Association of Dermatologists (BAD) reports a consensus view that the time required to synthesise vitamin D in the skin is relatively short, and less than the time needed for skin to redden and burn.
Importantly, continued sun exposure does not result in ongoing vitamin D production; vitamin D is converted into inert or inactive substances in the skin after prolonged UVB radiation. There is, therefore, no benefit in sunbathing for long periods of time purely to increase vitamin D levels.
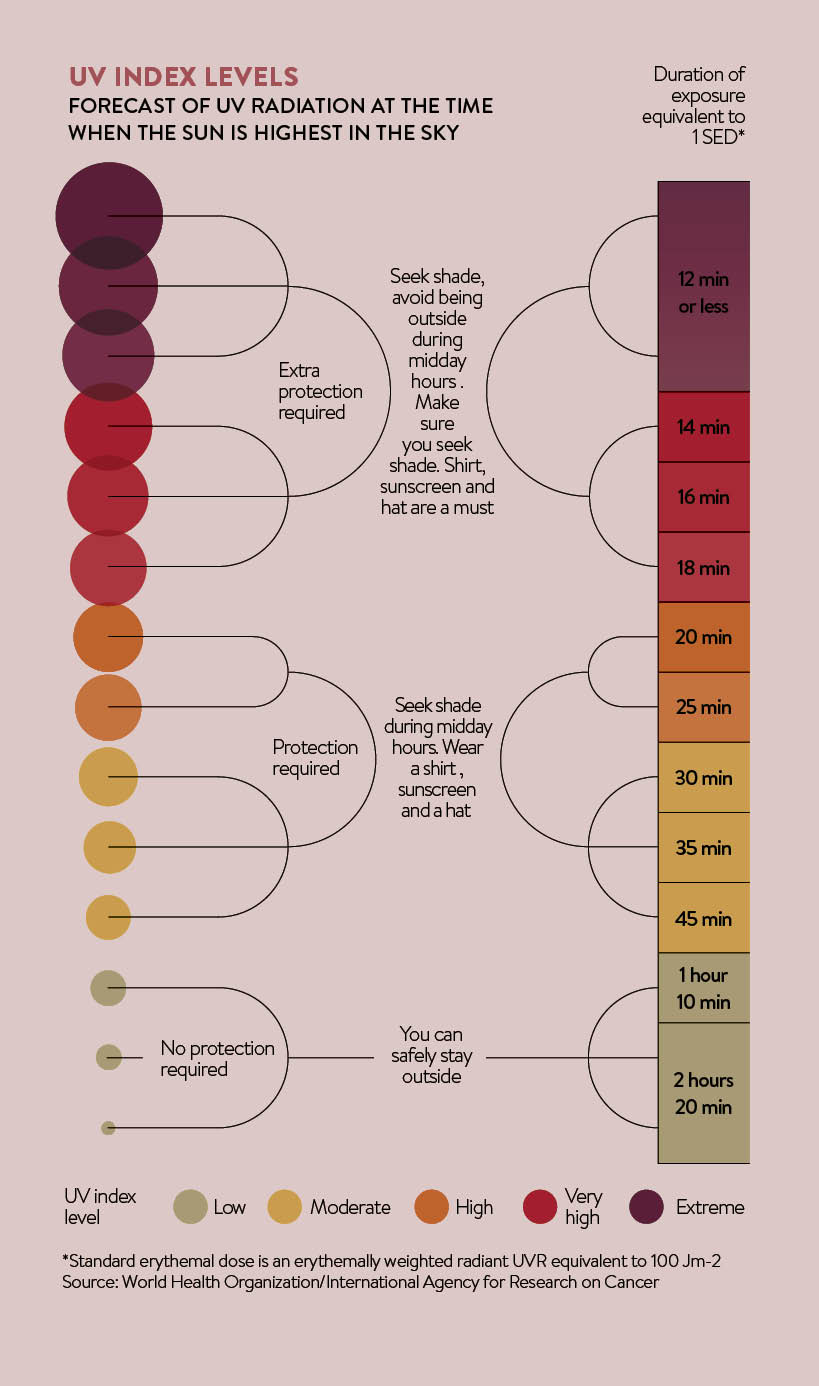
BAD’s guidance recommends being outdoors for a few minutes around midday without sunscreen, though individuals are encouraged to recognise their own skin to get some idea of how long they can spend outdoors without burning.
Other source of Vitamin D
Apart from sunlight, vitamin D can also be obtained from dietary sources and supplementation. Foods rich in vitamin D include oily fish, such as mackerel, salmon and sardines, as well as fortified margarine, cereals and egg yolks. Dr Hamdulay advises you should ensure adequate oral intake of vitamin D, recommended at 800 units a day, to reduce the risks of deficiency.
Oral vitamin D supplementation is likely to be necessary at times. Indeed, recent National Institute for Health and Care Excellence guidelines state that it is not possible to get enough vitamin D from sunlight between October and March in the UK. The Department of Health already recommends supplementation for pregnant and breastfeeding women, young children, older people and those at risk because of low sun-exposure.
It is worth noting that over-supplementation should also be treated with caution; high levels of vitamin D – above 75 nmol/L – have been linked to health problems. The key, as with everything, seems to be moderation.
Key concerns
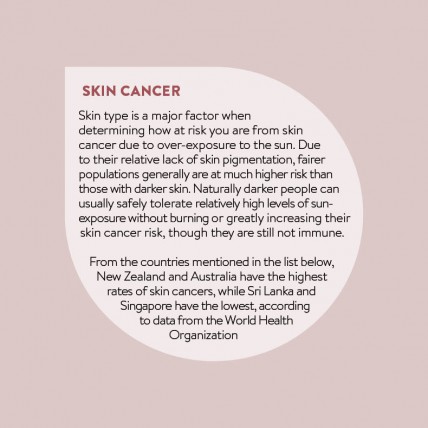
What is it that makes dermatologists so concerned about the sun? The fear is the rising rates of skin cancers, in particular melanoma, which is a potentially fatal skin cancer that occurs due to the uncontrolled growth of pigment-producing cells known as melanocytes.
It either develops within a pre-existing mole or manifests as a new mole on the body. It is the second most common cancer in those aged between 15 and 34. Data from Cancer Research UK confirms that rates of melanoma have continued to increase since the 1970s. This is likely to be related to the desire to look tanned together with the falling cost of holiday travel to sunny climates.
An estimated 86 per cent of melanoma cases are related to sun-exposure. Multiple sunburns, particularly in childhood, fair skin, outdoor occupations or hobbies, and sunny holidays abroad involving intermittent, high-intensity sunshine are all risk factors. While most melanoma is detected early and surgery is usually curative, survival rates remain poor for late-stage disease. Limiting sun-exposure is the most effective way to reduce the risks.
The British Skin Foundation recommends the use of regular sunscreen throughout the year to protect against skin cancer. This should ideally be at least sun protection factor 15, and provide broad-spectrum cover against UVA and UVB radiation.
How to protect your skin
Sunscreen should be worn on sun-exposed sites and applied at least 30 minutes before going outdoors. It should be reapplied about every 90 minutes and after sweating or swimming. An ounce of sunscreen is adequate to cover an adult from head to toe; this is approximately the amount contained in a shot glass. Half a teaspoon should adequately cover the face and neck.
Healthcare professionals are realising the importance of screening and early detection of skin cancer. Melanoma, when identified early, has a good prognosis. The skin is the largest organ of the body and any changes are outwardly visible, with no real requirement for detailed internal investigation. Skin, therefore, lends itself well to worrying changes being detected by a doctor.
Some people may wish to make mole-screening a part of their preventative health check
If you have any concerns about a mole, your GP is able to check it for you free on the NHS. If there is any possibility of skin cancer, the doctor will refer you to a dermatologist and you should be seen within two weeks.
Some people may wish to make mole-screening a part of their preventative health check. There are mole clinics available in the private sector, but according to BAD’s website, there is no evidence these “can replace the experienced clinical opinion of a trained consultant dermatologist”.
Dr Nisith Sheth, consultant dermatologist at the Lister Hospital, Stevenage, confirms this. “Mole-mapping with photographs can be a useful adjunct combined with a dermatologist examining the skin,” he says. “Photos can provide a useful record over time for any changes that occur.”
He advises being wary of any system where a dermatologist does not physically look at your skin. “Individuals should also get into the habit of looking at their own skin once a month to look for any changes and to seek medical attention if there is any doubt.”
There is evidence that rigorous sun protection can lead to vitamin D deficiency. Most dermatologists are nevertheless in agreement that the dangers of sun-exposure outweigh the benefits.
Vitamin D can be sourced from diet and supplementation if levels are low, rather than relying on the sun as a source to drive synthesis. There is no recognised health benefit of over-supplementation, however, and high levels may cause harm. The greatest risk of sun-overexposure is melanoma, a skin cancer that manifests as abnormal-looking moles. Any unusual moles should always be examined by a GP or dermatologist.
The benefits of Vitamin D