If it were a sales chart, the steep rise in people living with diabetes would send a boardroom into paroxysms of joy. Exponential growth is a rare phenomenon; in diabetes, it is a tragedy.
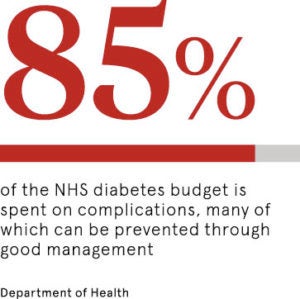
The consequences of a population shuffling through obesity mileposts are measured in human misery and soaring metrics that any business can understand. Treating diabetes costs the NHS £10 billion a year now; it will cost £16.9 billion, or 17 per cent of the NHS budget, by 2035 when the number of people with type-1 and type-2 diabetes will rise from 3.8 million to 6.8 million.
Despite dire warnings and klaxon lifestyle advice, along with the high profile of today’s World Diabetes Day focus, the number of people attending courses designed to help them manage the condition is disturbingly low. The charity Diabetes UK reports that just 41 per cent of people with type-2 diabetes and 19 per cent of people living with type-1 in England and Wales are meeting their targets for blood pressure, blood glucose and cholesterol.
Diabetes self-management education helps people stay healthy, live well, and reduce the risk of expensive and life threatening complications
Diabetes education measures are in place, but are they enough?
The results of poor condition management send shockwaves across society and the NHS, which performs more than 7,000 amputations a year, cares for 68,000 people with foot and leg ulcerations, and deals with a slew of other associated health problems caused by diabetes.
Guidance from the government health body NICE recommends that everyone diagnosed with diabetes should be offered free health education, yet figures show that just 2 per cent of people newly diagnosed with type-1 diabetes and 6 per cent of people with type 2 have attended a course.
World Diabetes Day is always an inspirational springboard for new treatments and technology, but education is a vital component in both preventing and controlling the disease.
“Diabetes self-management education helps people stay healthy, live well, and reduce the risk of expensive and life-threatening complications. People with diabetes are entitled to various free education courses, tailored to suit different needs,” says Nikki Joule, policy manager at Diabetes UK.
National courses are available, but attendance is influenced by poor referral rates, long waiting times for places, transport issues and the complex psychological payload that comes with a diagnosis.
Patients need to be trained on how to live with diabetes
Bernie Stribling of the Leicester Diabetes Centre and national director of the DESMOND course for type-2 diabetes, echoes concerns. “People with diabetes have a demanding condition to manage, yet on average they get to share this with a healthcare professional for an hour a year only,” she says.
“One hour of support out of a total of 8,766 a year to help them manage a condition which, if neglected, could lead to blindness, a lost limb, or an increased risk of a stroke or heart attack; that’s 525,900 minutes that a person has to draw on their own resources to manage their condition.
“People need to be given the essential knowledge and skills to manage their diabetes, otherwise they will be at risk of complications, including blindness, amputation, heart disease or stroke.
“Self-management education programmes that meet the national quality standards are a proven way of supporting people to self-care in diabetes. We believe this kind of diabetes education is key to preventing the looming NHS crisis and misery of the complications of the condition.”
Dr Campbell Murdoch, a Royal College of General Practitioners clinical adviser and chief medical officer at diabetes.co.uk, adds: “People need to know the risks, but equally be clear about the hope and the positive journey they can go on. They need knowledge, which is evidence based and up to date, and I don’t think it is available in certain areas of the country.
“My message to patients is that this is an important diagnosis that carries risk if you ignore it. But acknowledge it, harness a lifestyle and you can enjoy a healthy life.”
Digital diabetes education could be the answer
Digital education courses are available for type-1 diabetes and the NHS England’s transformation fund has just approved a new wave of online courses for people with type-2 diabetes.
Philip Newland-Jones, lead pharmacist for NHS England Diabetes and Endocrinology Clinical Reference Group, believes online courses, combined with new powers for community pharmacists to refer patients to structured education, would generate a dramatic increase in attendance and awareness.
“In some areas 80-plus per cent of patients are referred for education, but many don’t turn up because the waiting time for a place can be up to eight months, and they have been on Google and have lived with the disease for a long time by then.
“But there is an opportunity to dramatically improve the number of people accessing education and help.”
Mr Newland-Jones, consultant pharmacist in diabetes and endocrinology at Southampton Hospital, adds: “We have a pilot scheme, West Hampshire Diabetes Service, which could lead the way. Urgent referrals for episodes of low blood sugar are sent directly from community pharmacists to the community diabetes specialists, rather than having to refer through a GP. If this were to be extended to structured education referral and rolled out nationally, it would undoubtedly increase access to education for people with diabetes.”
Diabetes UK is calling for more flexible times and better course locations to boost access alongside the digital impetus.
“As the number of people with diabetes grows, it’s vital that access to diabetes education is improved,” concludes Diabetes UK’s Ms Joule. “The NHS must continue to build on the progress already made and continue the diabetes transformation funding beyond 2019 to ensure that as many people as possible have access to the diabetes education they’re entitled to.”
Diabetes education measures are in place, but are they enough?
Patients need to be trained on how to live with diabetes