When Yorkshireman Tony Green was struck down with sudden chest pain aged 57, he thought he was having a heart attack. He called an ambulance, but despite quick treatment and a hospital ECG scan, doctors could find nothing wrong.
The next two years were a frightening time, as Tony, a Sky TV investigations consultant now living in Glasgow, suffered frequent similar attacks.
He says: “It was very scary – the attacks were coming at regular intervals without any warning, the pain was getting more intense and to be out of control is a horrible way to live.”
Tony was finally diagnosed using a new credit-card sized heart monitor called a KardiaMobile, which records the electrical activity of his heart through his fingertips.
He was found to have atrial fibrillation, an irregular heart rhythm disorder, which was not being picked up in hospital tests because of its transient nature. Finally, he was put on effective treatment.
Tony, now 60, says he feels normal again and is actively involved in his healthcare, carrying the KardiaMobile everywhere. “It’s really easy; you open the app on your phone and put your fingers on the pad – that’s how simple it is. You just email the readout to your GP or, in my case, my cardio consultant,” he explains.
Since February, the device is now being rolled out as part of an NHS England-funded project, via the country’s Academic Health Science Networks and is one of the latest examples of patient-centric technology that is set to transform healthcare in 2018.
Francis White, vice president of makers AliveCor, says it enables patients to capture and understand their own health information, in this case heart rhythm, wherever they are, which is empowering.
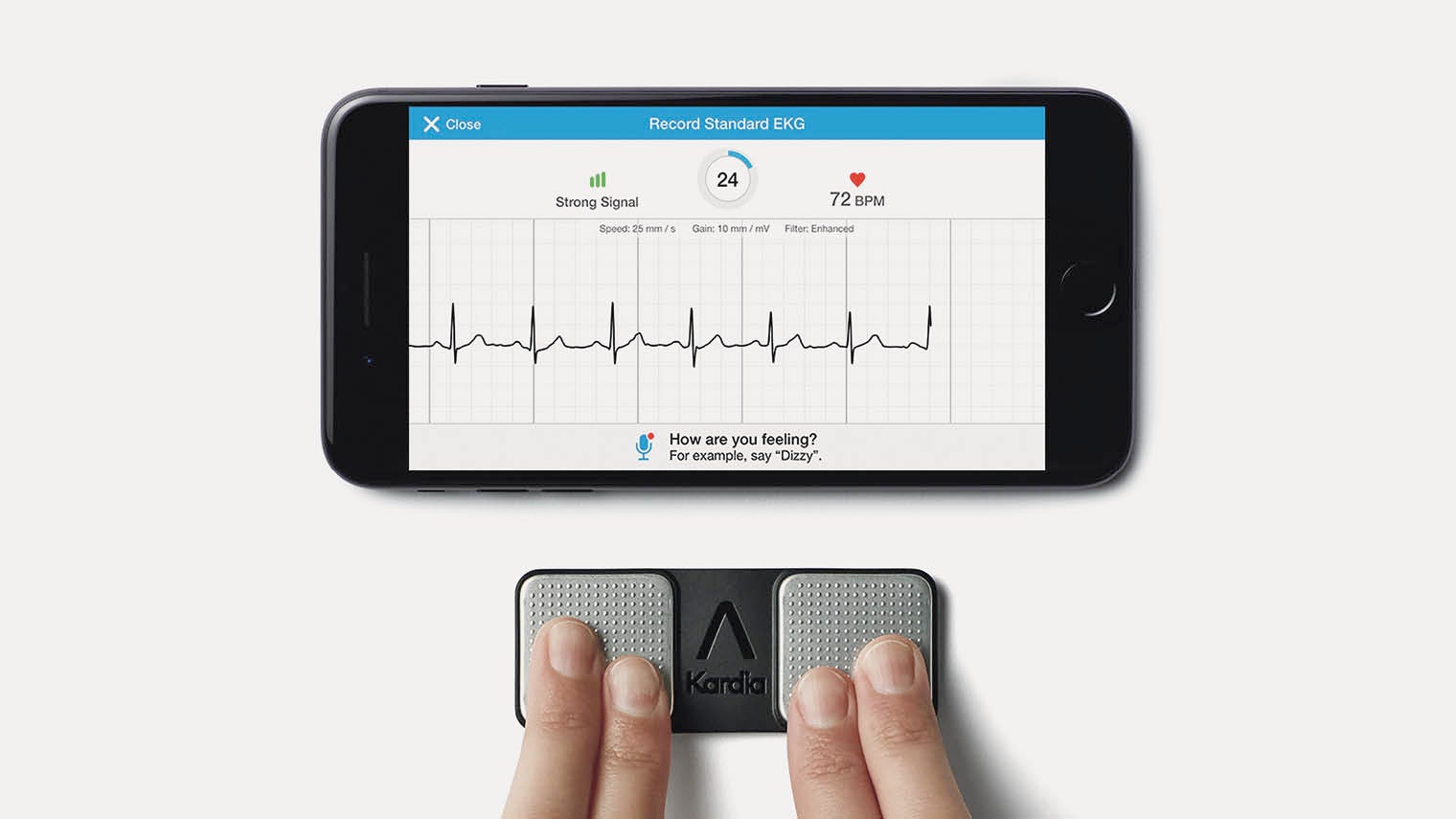
AliveCor’s KardiaMobile app and medical-grade ECG empowers customers to detect an abnormal heart rhythm and share the information with their doctor
He says: “We involved patients from day one, working with the Atrial Fibrillation Association in the UK. We gave them hundreds of devices so their members could give us feedback and that learning was unbelievable powerful for us.”
This involves a shift from patients being passengers to drivers of their health, with responsibilities too
Patient-centred healthcare is about patients being involved in decisions about them, rather than something that is done to them by a doctor. This involves a shift from patients being passengers to drivers of their health, with responsibilities too.
Patient-centric technology is about creating tech designed very much with the patient in mind and how they are going to use it. Both are deeply wrapped up with the concept of individualised, personalised treatment and care.
Dr James Somauroo, former NHS anaesthetist and critical care doctor, founded accelerator company HS, with three other colleagues, which builds and scales healthcare startups.
To be considered, candidates have to show evidence of patient centricity. Successful applicants include Qdoctor, a telehealth service for NHS GPs, which enables clinicians to provide continuity of care for their patients with video consultations in and out of hours, and XenBot, a chatbot which boosts mental health by helping people journal their thoughts through introspective questions.

Motorola’s Vital Moto Mod is a snapon extension to the Moto Z smartphone that measures heart rate, respiratory rate, body temperature and both systolic and diastolic blood pressure
Dr Somauroo says: “I firmly believe that healthtech startups and companies need to be connected with patient groups from the get-go. It is vital that health companies focus early product development around building something that patients love to use, and that offers a convenient and effective way to improve their health.
“Any product which directly affects the patient should be built with patient-centric feedback and development at its heart.”
Patient-centric healthcare is gaining momentum on a range of levels, making healthcare more comfortable, more convenient and more accessible, thanks to feedback from ordinary people.
For years, women have complained that the breast compression needed for mammograms can be painful. Now a new pain-free ultrasound screening method is being developed in the UK to detect breast cancer, which would eradicate the need for compression.
In terms of convenience, repeated hospital visits for chronic conditions are a bugbear. To combat this, Lancashire Teaching Hospitals NHS Foundation Trust has teamed up with video-conferencing experts Polycom to enable kidney patients living in a 100-mile radius to have home dialysis treatment via a video link. After appropriate training, nurses supervise remotely and can zoom in on procedures and provide the highest level of expertise.
The new system gives patients, who previously had to travel miles several times a week for lengthy treatment, more freedom as well as the chance to collaborate and be engaged in their treatment.
Patient centricity is not limited to treatments or interventions. Plymouth Hospitals NHS Trust is working with networking experts Aruba to help enhance patient experience by making sure they have access to the internet, which ultimately will help to improve care.
Despite a “hostile” environment for internet connectivity, with 12 uniquely shaped floors and massive amounts of pipework and electrical equipment, Aruba has enabled an extensive wired and wireless system for staff, visitors and patients. This means that 2,500 mobile devices are connecting every day, with around 70 per cent of the wifi used by patients.
The trust also has 250 iPads around the site, set up for patients to take the “Friends and Family” test on whether you would recommend loved ones to be treated there, information that is then being fed back to improve services.
Experts agree that with the proliferation of digital technology and demand for personalised treatment, a focus on patients will make the difference between success and failure.
Dave Challis, vice president of health innovation at consumer giant RB, says that as the health market becomes saturated with products offering similar services, many emerging solutions will disappear as fads. But he concludes: “Those that deliver real benefits to consumers and are truly patient centric will succeed.”
