A genome is the body’s instruction manual. It’s made of DNA and there is a copy in almost every cell.
Through genome sequencing and genomics, clinicians can better understand how cancer cells might evolve and what treatments will be most responsive, known as precision and personalised medicine.
Furthermore, genomics combined with technologies such as machine-learning and artificial intelligence (AI) has huge, as yet untapped, potential for determining a healthy person’s future risk of cancer.
Genome sequencing means we can get all the information needed from one test, whereas previously several were required
New government goals for genome sequencing
To sequence the first genome cost $3 billion and took 13 years. But today, Illumina, the NHS’s technology partner, can do it for a comparatively mere $1,000, a price drop that is driving innovation in the field.
Building on its groundbreaking Genomics England initiative to sequence 100,000 genomes, earlier in the year the UK government announced a new Genomic Medicine Service is being rolled out for children and adults with rare diseases and some types of cancer, so doctors can provide more personalised treatment.
Health secretary Matt Hancock said recently the aspiration is to sequence five million genomes over the next five years.
“Genome sequencing means we can get all the information needed from one test, whereas previously several were required,” says Professor Trevor Graham from the Barts Cancer Institute at Queen Mary University of London.
He is conducting early-stage research funded by Cancer Research UK using computers, mathematical modelling and genetic data to piece together a cancer’s history to predict how tumours evolve.
Using new tech to make genome data accurate
To derive insights from the huge amount of information a sequenced genome produces, clinicians are seeking help from advanced data science techniques.
For example, SOPHiA GENETICS’ SOPHiA AI software-as-a-service (SaaS) platform uses algorithmic technology to make genomic data more accurate for diagnostics by cleaning and standardising it, removing anything that could present bias or false results, which is a frequent problem. It then highlights variances in the data that could be causing the cancer and provides treatment suggestions.
“It is up to the clinician to make the final diagnosis about pathogenicity and treatment, but SOPHiA can provide a prediction, as well as identify specific treatments on the market and even link patients to potential ongoing or upcoming drug discovery trials,” explains Iole Pezzuto, scientific communication specialist at the company.
The technology is used in 800 hospitals worldwide for hereditary disorders, including cancer, and oncology for both solid tumour and haematological disorders. In September, it opened a US headquarters.
Genome sequencing data used to aid prevention
To celebrate this October’s Breast Cancer Awareness Month, the company made public new technology that uses similar techniques to help quantify a patient’s risk of cancer.
Known as PREVENT, the test is based on ten years of studies. It combines genome sequencing data, provided by a simple mouth swab, and information about lifestyle, including smoking, weight and fitness, with non-modifiable factors, such as age, which is fed into an algorithm to create an individual’s risk score.
Dr Jonathan Krell, consultant medical oncologist at Imperial College London Healthcare NHS Foundation Trust, has been trialling the PREVENT technology. He says it has the potential to improve breast screening programmes, so women are checked when they actually need it.
Presently, women are only routinely screened from the age of 50, even though 50 per cent of breast cancer patients are actually younger.
“This technology can help us determine who should be undergoing breast screening at age 35, for example, but who doesn’t need it until they are 80,” he explains. “From a public health and economic perspective, this will have a huge impact in personalising our screening programmes, because right now it is not good enough to say we screen by age eligibility alone, as that is not the only risk determiner.”
The PREVENT model could potentially work for any cancer, but is especially useful for those where there is an effective way to screen patients, for example, with mammograms or blood tests.
Technology companies are focusing their efforts on combining genome testing and advanced data technologies for more precise cancer treatments, diagnosis and drug discovery
More technology companies getting involved in healthcare
Dr Krell thinks patients could be regularly tested to determine their level of risk and, if necessary, offered preventative surgery or medicine.
“I absolutely believe in the future we will be using platforms like PREVENT in a similar way to how we provide immunisations or check blood pressure and diabetes today,” he says.
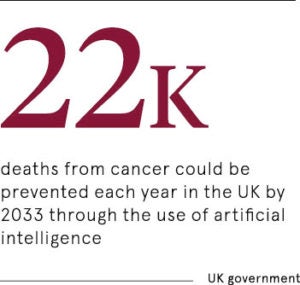
Prevention and early diagnosis is a growing focus for both companies and healthcare providers. The UK government has said it wants the NHS to detect three out of four cancers at an early stage by 2028. Patients diagnosed early, at stages one or two, have the best chance of long-term survival.
Patients, of course, will want this too. PREVENT, according to Dr Krell, was inspired by home genetic tests like 23andMe, which can provide more than 90 personalised reports about a person’s ancestry, health and wellness, through a saliva sample.
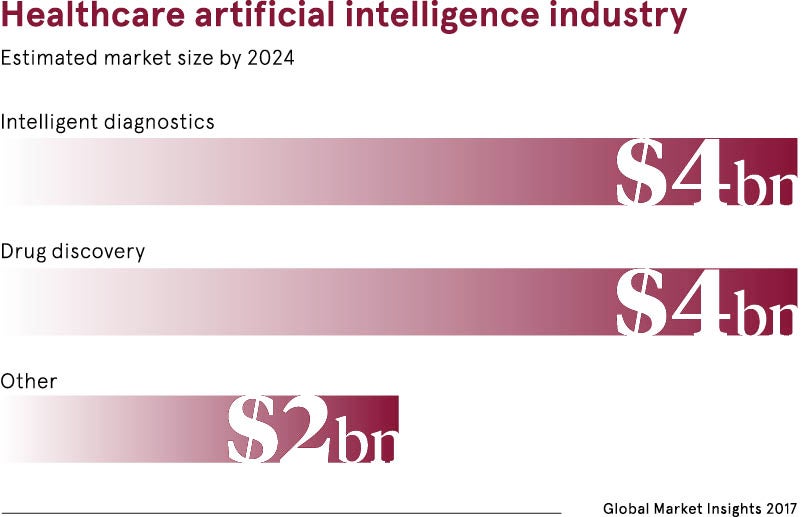
In fact, more and more technology companies are focusing their efforts on combining genome testing and advanced data technologies for more precise cancer treatments, diagnosis and drug discovery.
Last December, Google released DeepVariant, an open source deep-learning model that has been trained to analyse genetic sequences and accurately identify variants.
Furthermore, Canadian-based Deep Genomics is developing what it calls an AI-driven platform that supports geneticists, molecular biologists and chemists in the development of new therapies.
Genomics offering exciting opportunities for the future
“Looking at an individual’s genomes and calculating their risk of cancer, and diagnosing tumours based on its molecular genetic make-up, instead of where it is located on the body, is exciting,” says Professor Graham. “So is big data and analysis, and it is made possible by the very large access we now have to different sets of data like Genomic England.”
Most of these technologies, once approved by a national public health body, are fairly easy to adopt in the clinical setting, because they only require sending away samples or integrating a SaaS programme.
Dr Krell concludes: “There are limitations, but they are great ways of improving how we analyse data. They are expensive, but they will be worth it in the long term.”
New government goals for genome sequencing
Using new tech to make genome data accurate