Connecting health and social care is a necessary 21st-century evolution of overburdened services.
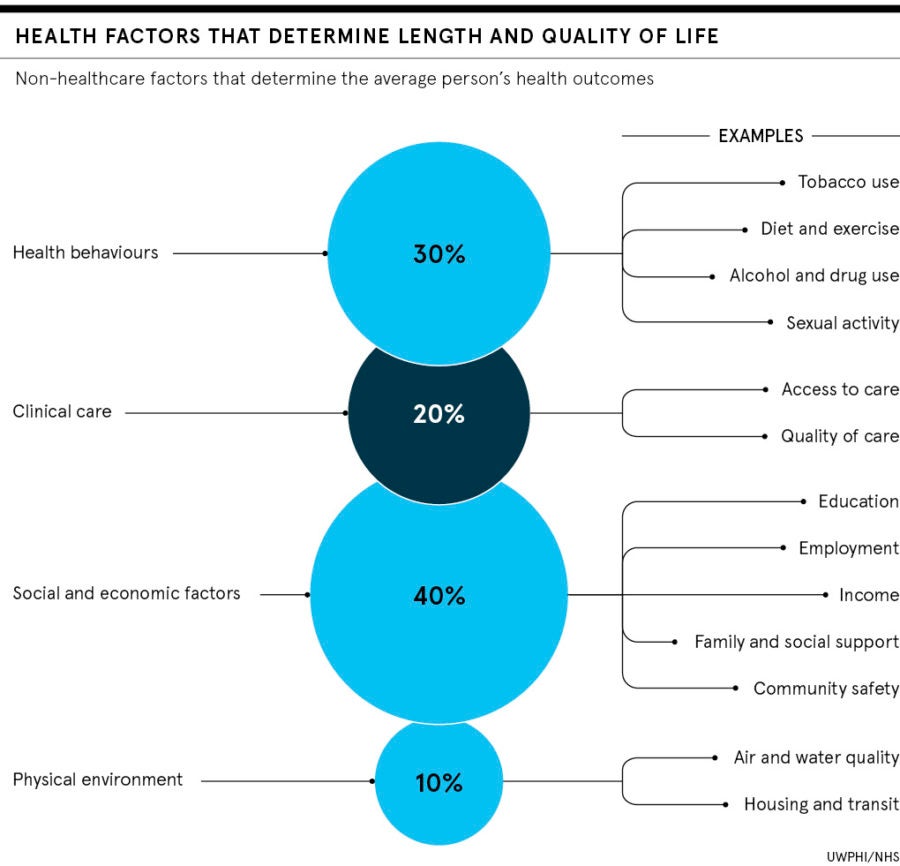
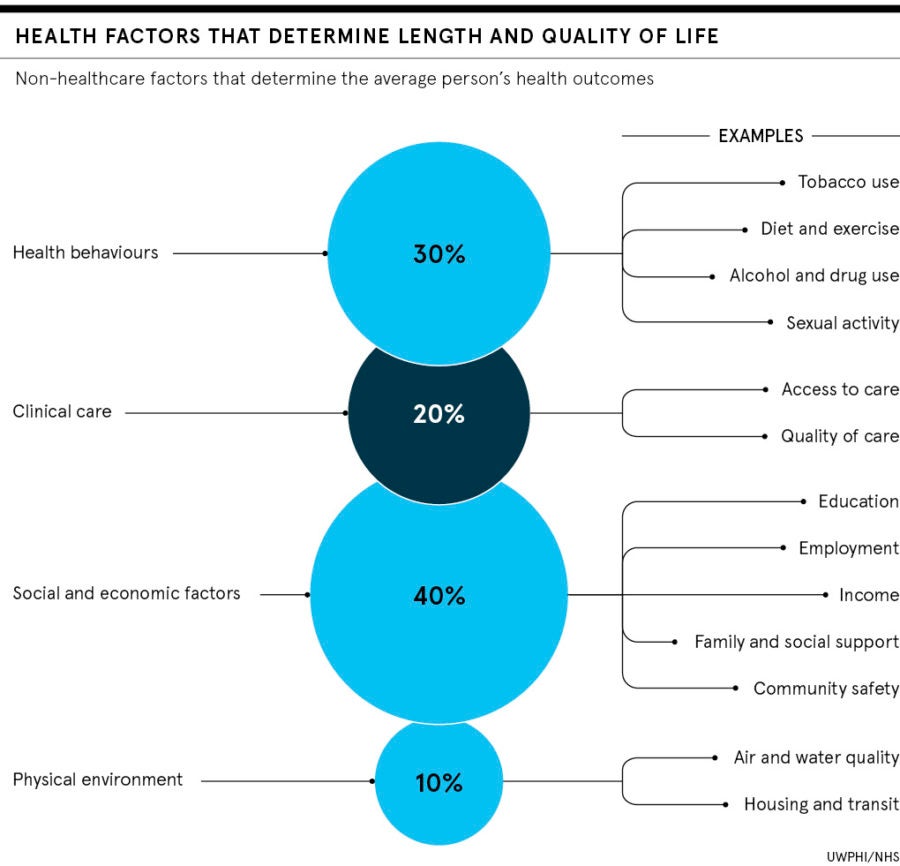
Just 20 per cent of a person’s health outcomes rely on medical care; housing, education and other social factors collectively influence the remaining 80 per cent. Joining up domiciliary care, mental health services and healthcare, through digitalisation and sharing data, creates a continuum of care, but is only happening in pockets.
A wave of cheap, consumer-based technology is becoming available on mobile devices, bringing the opportunity to deliver better care in people’s homes, promote wellbeing and avoid expensive hospitalisation.
A smartphone can measure pulse, respiration, blood pressure and blood oxygen, and even do ECGs. Miniaturised, mobile technology is shifting care out of hospitals and surgeries, and connecting networks of professionals around patients.
Community interest company Care City equips domiciliary care workers and even shop assistants with mobile digital technology to promote healthy ageing and social regeneration in East London.
“Diagnostic technology is developing fast, is cheap and portable, and already in the pocket. That’s exciting for health and social care as the diagnostic brains are in the cloud,” says John Craig, Care City chief executive.
Consumer tech delivers cross-functional care
In a Care City pilot, part of the Innovation Test Bed run by NHS England and Office for Life Sciences, care workers with mobile devices take observations that are run against an algorithm using the so-called national early-warning score. If the screen turns red, from green, the care worker escalates to a health worker who uses the data to make a clinical diagnosis, saving resources and keeping people out of hospital.
This exemplar, happening in homes in Barking, is proof of how digital innovation at the edge can connect relevant care professionals with patients in their homes. Integrating data, IT systems and governance to provide joined-up patient journeys at scale, however, is a far greater task and Manchester is arguably the most advanced region.
Around the country, 14 regions are building integrated care systems and Manchester has used its devolved local government status to form the Greater Manchester Health and Social Care Partnership.
Dr Tom Tasker, local GP and chair of the joint commissioning board, says local government agencies no longer pull in different directions with different budgeting priorities. “Health and local authority commissioners together provide the best value for the Salford pound,” he says.
Connecting agencies improves health outcomes
The healthcare model that the partnership embraces is broad, connecting multiple agencies, including schools, mental health and children’s services, in support of Manchester’s mantra: “Start well, live well age well”.
Mayor Andy Burnham’s A Bed Every Night initiative to counter homelessness has bucked the national trend, reducing rough sleeping by over a third in the past year. Wrapping health interventions, care packages and housing together has been a key factor in the success story, says Tasker.
Integration on this scale is an immense task. But social enterprises and technology firms, working with local authorities and clinical commissioning groups (CCGs), are proving that joining up small datapoints along the patient journey also pays. At Leeds Teaching Hospitals NHS Trust, mobile computer vision supplier Scandit trialled barcode scanning on digital devices as part of the NHS Scan4Safety pilot, designed to boost compliance of drug administration and patient safety.
Care workers can escalate to health workers who use data to make a clinical diagnosis, keeping people out of hospital
By linking information on patients’ wristbands, encoded with a standard barcode, with an electronic patient record and patient administration system, Leeds now has a near real-time view of the patient journey. Such transparency is valuable in costing treatment, improving clinicians’ practice and realising significant financial savings.
Joining data to reimagine care experience
Progressive health and social care administrations are harnessing data transparency and business intelligence (BI) as a radical force in reimagining citizen care. West Cheshire CCG is building an intelligence-led organisation. Starting point was a data stratification tool that predicts risk of hospital readmission. The BI team also wanted to identify people at risk of first-time admission, says Andy McGivern, associate director of BI for Cheshire CCGs.
Realising the ambition called for social determinants to be collated and much time was spent talking to the council and achieving data-sharing agreements. Joining up data about patients’ locations, admissions, diagnoses, observations, mental health and primary services, prescription data, and 111 calls created new profiling capability.
“Providers thought they knew their high-risk patients, but they only knew 60 per cent. The data surfaced the other 40 per cent of patients at risk of admission,” says McGivern.
While politicians, commissioners and practitioners grapple with systemic integration of finance, governance and IT systems, digital is connecting health and social care in novel ways.
Refero, a secure engagement platform, is putting vulnerable and excluded young people at the centre of their own family and professional support network in south-west England. Video conferencing tools, such as LIVI and vCreate, are helping GP surgeries and hospital wards stay connected with patients and families.
Former government tsar for emergency care Professor Matthew Cooke concludes: “New technologies enable records to be more secure and to restrict access to those who need to know.” Digital systems can help provide seamless care across health and social care, but as Cooke sums up: “It’s work in progress at present.”
Consumer tech delivers cross-functional care