Mention the word fertility and most people immediately think of women and mums. Yet the reality is very different. Male infertility is the cause of problems in heterosexual couples in half of all cases. Men are finding it more difficult to become fathers because sperm counts are falling.
There has been growing evidence of this over a period of years. A landmark study of thousands of men over 40 years, published in 2017 by the Hebrew University of Jerusalem, showed a significant decline of more than 50 per cent in sperm counts in Western men, with no sign of this decline levelling off.
According to lead author Dr Hagai Levine: “Given the importance of sperm counts for male fertility and human health, this study is an urgent wake-up call for researchers and health authorities around the world to investigate the causes of the sharp ongoing drop in sperm count, with the goal of prevention.”
Despite how common male fertility problems are, there’s nothing we can prescribe or add to sperm to cure it
The study provided conclusive evidence of the decline in sperm count, but it did not seek to identify the causes. Even now, the reasons for the fall remain elusive. There is some evidence that it is caused by environmental factors, such as exposure to chemicals through what we eat and drink, or the poor quality of the air we breathe in towns and cities.
But more research is needed before we can be certain. However, the low priority given to male fertility continues to inhibit the scale of research into both the causes and the treatments.
Male infertility testing and treatment have changed little over the years
Treatment for male infertility has changed very little over the years and is still largely provided as an extension of female infertility, to be accessed when treatment for the female partner has not resulted in conception.
The standard NHS semen analysis hasn’t really changed in decades, looking at a sperm sample under a microscope to assess three key parameters: sperm count, motility (can they swim?) and morphology (are they the right shape?). But semen analysis is an imperfect process. If you have a normal, or even high, sperm count, it doesn’t guarantee you are fertile, while if you have a very low sperm count, it doesn’t guarantee you are infertile.
Professor Sheena Lewis, chairwoman of the British Andrology Society, which aims to improve care in men’s reproductive health, says addressing the lack of focus on male infertility within the health system is an urgent problem. “Men are not being looked after properly, not diagnosed and not cared for,” she says. “The woman actually acts as the therapy for the man’s problem. We are giving an invasive procedure to a person who doesn’t need it, in order to treat another person. That doesn’t happen in any other branch of medicine.”
A man diagnosed with a fertility problem is likely to be referred to a specialist in women’s reproductive health, with little or no training in diagnosing or treating male patients. Gynaecologists don’t perform physical examinations on men to check for any testicular issues that could be affecting fertility, which might be easily resolved, or consider a full clinical history to identify an underlying health problem or problematic lifestyle factors. And his partner is still likely to undergo a number of investigations, even though she may not actually have fertility issues.
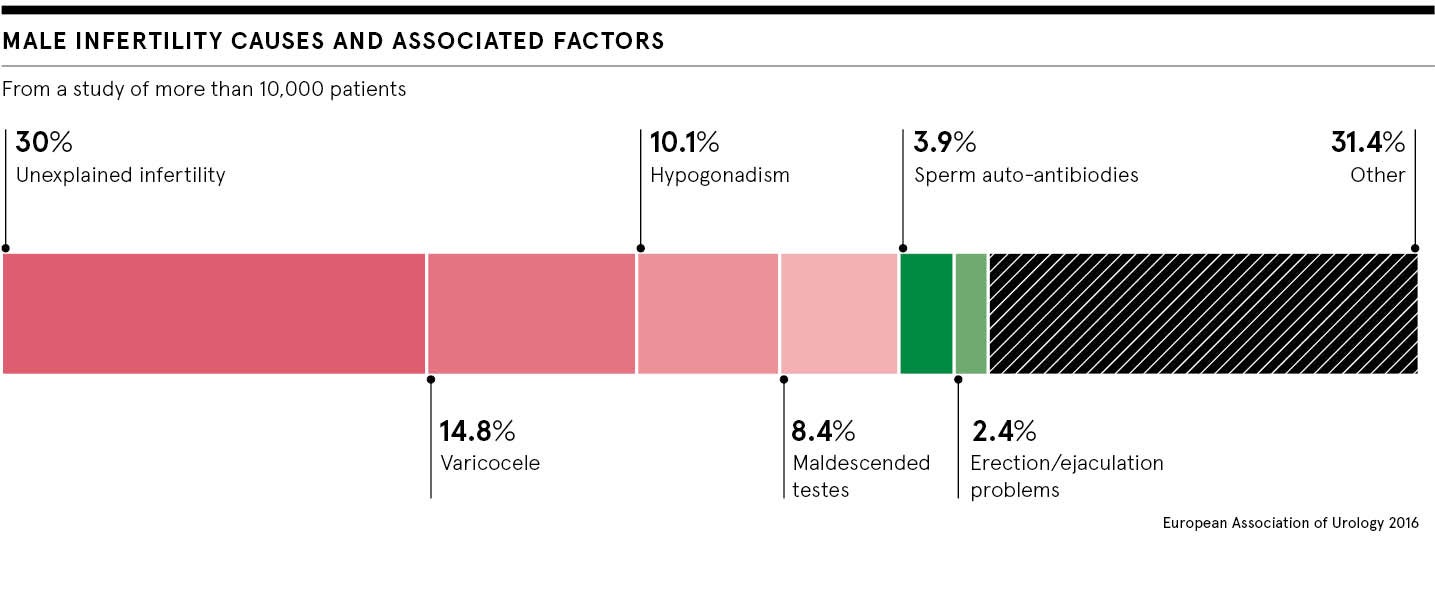
What factors affect male fertility?
Dr Sarah Martins da Silva, who runs a research programme at the University of Dundee focused on sperm biology and drug discovery for male sub-fertility, says: “Despite how common male fertility problems are, there’s nothing we can prescribe or add to sperm to cure it. Couples rely on fertility treatment such as IVF, which is expensive and doesn’t guarantee success.”
What we do know is that men certainly cannot take their fertility for granted. Testicles contain sperm and protect the delicate cells from the outside environment. Damage to your testicles can have a serious impact on your fertility by affecting the quality and quantity of sperm.
Overheating sperm can seriously impact their quality. Keeping testicles cool is important to maintain an optimum temperature of the sperm. Simple ways to do this include avoiding sitting down for long periods and not wearing tight underwear. Other causes of testicular damage are trauma, such as from sport, infection, testicular surgery, a congenital defect or undescended testicles.
Having problems with ejaculation can impact fertility if sperm cannot reach the egg for it to be fertilised. Examples of ejaculatory disorders include premature ejaculation, retrograde ejaculation, where semen is ejaculated into the bladder, as well as failure to ejaculate.
Male fertility needs to be made a greater priority
Healthy lifestyle choices are among the most important and manageable ways to improve fertility. Sperm quality, quantity or sperm passage may be adversely affected by excessive alcohol, steroids, illegal recreational drugs, such as cocaine and marijuana, an unhealthy diet and obesity. Unsafe sex can lead to sexually transmitted diseases that can block the sperm passage.
Male fertility is becoming a genuine public health issue and should be given greater priority by health authorities. Men also need to be aware that just as they share responsibility with women for birth control, they cannot leave fertility concerns to women. Men can also be the problem.
Male infertility testing and treatment have changed little over the years