NHS commissioning support units (CSUs) are an essential part of the health and care infrastructure, helping plan service delivery and ensuring efficient resource usage. Each covers a region containing thousands of GPs and dozens of hospital trusts, as well as countless other health and care organisations, which rely on their CSU for a wide range of services and support. They also play an essential role in identifying and helping reduce health inequalities in their areas. But how could this be affected by the increased digital delivery of healthcare?
Experts from three CSUs, whose combined footprint covers more than half of England, plus Paul Clarke, head of government practice at Esri UK, which provides advanced geographical information systems that can help identify patterns of health inequality or uneven service delivery, share their views.
What are the most important things learnt about inequalities and digital healthcare over the last 12 months?
MVH It has certainly brought inequalities into sharp focus. It’s also forced the pace on the whole digital-first agenda within healthcare and challenged some of our assumptions around, for instance, senior people not being digitally aware. We were aware of these issues, but they have now gone to the top of the list.
DB It’s emphasised what we’ve known about particular groups of the population being more likely to be affected by health inequalities due to socio-economic factors such as ethnicity and social deprivation. As part of our response to the pandemic, we have been trying to identify the factors that could have a disproportionate, negative impact on those who may contract the virus.
PC What has stood out for me is the existing indicators of health inequality, like access to transport, housing and socio-economic conditions, and ethnicity are the same factors that put people at risk from coronavirus. The last 12 months have also made clear how in the public sector the data is held in lots of places, some in the health service, the police service, some in local authorities and further afield. The pandemic has forced the agenda, bringing those organisations together to mount an appropriate response, solving problems that were thought insurmountable.
HS Yes, bringing a lot of those datasets together has enabled us to have a much clearer handle on the risk of having a worse outcome from COVID, including in areas with significant inequalities. Collectively, there is a lot of learning to be done from a data and a digital perspective.
On the issue of inequality, do we fully understand the issues? Or are there still unknowns?
HS We have established ways in the NHS to look collectively at how we segment the data to look at factors that disadvantage some populations. We’ve been able to put the learning from COVID on top of this to enhance that level of understanding further. But I think it will continue to evolve; there will always be unknowns. The issue for us is to keep working together, speed up the pace at which we increase our level of understanding. This is not a start-and-finish situation.
PC I often hear people saying their data is incomplete. If people have no faith in data, they have low care about what they capture and it can feed upon itself. They need information products that give them value, which in turn creates a business case for why they should capture it in a quality way. Better quality data with good spatial analysis tools will allow us to discover new patterns.
The pandemic has forced the agenda, bringing those organisations together to mount an appropriate response, solving problems that were thought insurmountable
DB What’s emerged during COVID, the positive community response to it, is the importance of tacit knowledge to enhance our understanding and inform the approach to tackling health inequalities. The question going forward is how do we effectively harness the tacit knowledge individuals and communities have.
Are we making the best use of the tools and data we already have?
MVH I think we’re making really good use of it, but we could do more. It’s about having a cultural openness to it. And sometimes you could say the tools can do more than people have the headspace to use. You can produce reports with fantastic information, but people sometimes don’t have the time to dig in and gain insight.
DB It’s all about interpreting data, converting it into actionable insight. If you’re presenting data differently, such as geospatial data or heatmaps, that can help.
MVH The point about geospatial information systems (GIS) is an important one. It allows us to visualise data in a way that people can really connect to; it means something to people and they can relate right away. We’ve seen huge growth in the amount of GIS work we’re doing and we’ve doubled our team in the last year or two.
PC We see excellent use of tools and data, but we can always do more. For example, we know that there are challenges about using data from individuals, how we ensure anonymity. But once you aggregate data geographically, it almost automatically anonymises it, making it safe to share. It also provides immediate interest to people because they can contextualise it: this is where I live, this is where I work and so on. It also allows you to bring lots of different datasets together. Suddenly you can aggregate information from the NHS, the local authority, data about air quality, with location as the reference, getting real insights.
HS You could be looking at two GP practices and find they have pretty similar demographics, but generate very different outcomes from episodes that come out of the pandemic, for example mental health or respiratory disease. You can then say: “OK, the demographics are similar; what’s made a difference?”. You can support ongoing discussion and debate.
MVH Another good example is mapping the low uptake of vaccinations and seeing if there is any particular geographical pattern. That’s been incredibly useful in drawing conclusions about why certain individuals aren’t getting the vaccine when invited.
Do we have the data we need to generate real insights?
HS We don’t want a whole smorgasbord of datasets that just gets bigger and bigger if that takes us away from doing our job, which is analysing the data, seeing the insights we can take from it and then doing what needs to be done locally.
Is the move to more digital delivery of healthcare, such as video outpatient and GP consultations, lasting?
MVH Some of the surge of progress we’ve had throughout COVID perhaps won’t be maintained, some has subsided already. But I do think there will be lasting change in the way people use data and making sure solutions such as clinical pathways are digitally led. I think it’s important to ensure equality, ensuring that digital is not the only way to access good care.
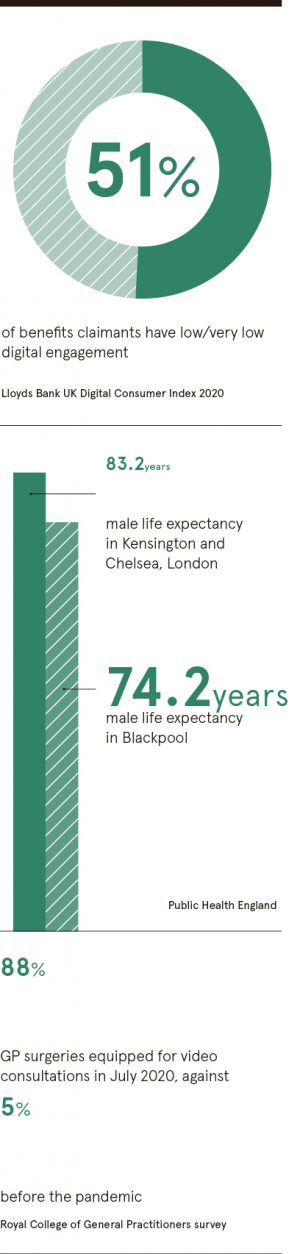
PC Not all members of the public are going to access services digitally. But using data to understand that and target people with appropriate alternative services is powerful.
DBI think it’s essential we do robust evaluations of digital programmes, so we understand the benefits and impacts they’ve had and we don’t just make a simple set of assumptions and assume it is the reality.
Data and digital can really help empower patients and citizens to take greater control of their health
HS I agree. It’s important to ask, has it done what it said on the tin? And this may require niche skills that might not normally be within the NHS. When we do analysis, I also think we need to be broader in our approach. It comes back to a storytelling perspective: this was the problem, this was the target group, this was the intervention and these were the results. This builds ongoing trust in how data is being used and the social benefit.
Who is at risk of not being able to access new, digital services?
DB There are multiple factors impacting digital take-up. One is willingness. But geographical variation is also significant. The communities I work with range from very urban to sparsely populated rural areas where many people struggle to get broadband. There are parallels to the families trying to access education during lockdown where some families had limited connectivity to the internet or due to financial hardship not everyone could afford a device, or were trying to access lessons using a pay-as-you-go mobile. It needs a multi-organisation response because there are multiple factors we need to work together to overcome.
Is now the moment for a push towards preventative medicine?
MVH This is something we have been focused on for quite a few years now. Much of the data integration leads us down that path and the pandemic, of course, has accelerated this. And so has the greater availability of digital information. So I think now is a pivotal moment in terms of the opportunity to do this efficiently.
DB Data and digital can really help empower patients and citizens to take greater control of their health. There are numerous examples of that, for weight management for instance, a personalised, targeted preventative support programme using data is very powerful.
HS I live in a rural area, so I often see walkers, but now I see a lot more, especially families. I would love to think we could capture data about that so you could see how it impacts general wellbeing rather than our more traditional ways of measuring things.
PC We were talking earlier about data and visualisation tools; I think there is an opportunity here as well. You can look at a location and ask why the outcomes are good. And you can look at another area and understand how a couple of points shift in behaviour will bring benefits. It allows you to target resources and share with the public—tangible and demonstrable benefits from taking action.
DB When I first joined the NHS 15 years ago, I recall having a conversation with a GP and one of his patients. She was an older lady who had a thyroid problem. She could access her GP record and test results and had agreed with her GP the thresholds that allowed her to manage that condition, adjusting her medication. She said it was truly transformative for her as a patient. These sorts of stories are very powerful because we can all relate to them.
To discover more please visit esriuk.com/health
Promoted by esri