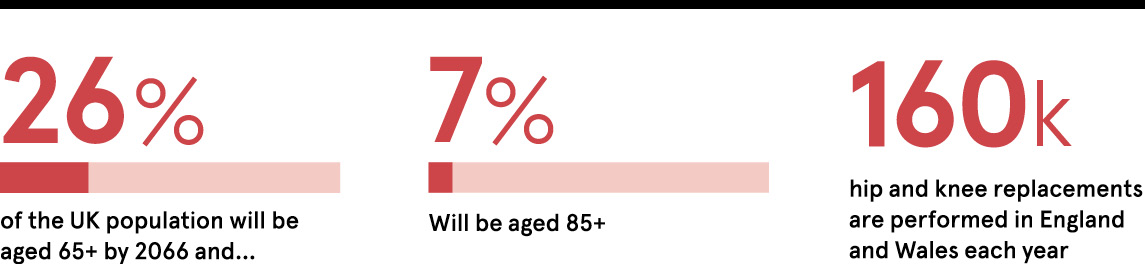
Common orthopaedic procedures, such as hip and knee replacements, which are performed approximately 160,000 times each year in hospitals across England and Wales, are being supercharged with technology that has the potential to improve patient outcomes, reduce operation times and save costs in the health service.
Dedicated research and development programmes from DePuy Synthes, one of the world’s largest and most comprehensive orthopaedic medical device businesses, are enabling advances for some of the most common surgical procedures performed in the NHS.
The demand for hip, knee and other joint surgery is growing as we experience demographic shifts that will see people aged over 65 making up 26 per cent of the population and the number of over-85 year olds trebling to 5.1 million or 7 per cent of the population by 2066, according to the Office for National Statistics.
The ageing population is already putting huge strain on NHS finances and logistics, but DePuy Synthes is committed to developing a broad range of innovations that drive practical solutions, such as 3D printing of orthopaedic implants and instruments, the use of robotics during surgery, and digital technologies to support education, surgeon training and patient engagement throughout their treatment.
“There is an exciting future ahead and we are laser-focused on improving outcomes for patients,” says Dr Mike Barker, the company’s worldwide vice president of research and development. “We are developing innovative solutions that deliver value. This means achieving both the best possible outcome for a unique patient, while also delivering overall efficiencies for the health service.”
DePuy Synthes, which has a large R&D centre based in Leeds and is part of the Johnson & Johnson family of companies, has a heritage in orthopaedics of more than 120 years. It has continued to innovate solutions and develop strong partnerships with major universities, key opinion leaders and technology startups to ensure its research and development offering is at the cutting edge of the medical devices industry.
For patients presenting with particularly complex cases, its 3D-printing advances are transforming challenging hip and knee replacement procedures by employing patient CT scans to 3D model the geometry of a patient’s joint pre-operation, and then designing and precision printing patient-matched metal implant or alignment instruments to ensure the best possible fit. This is creating treatment options for patients that were not previously available, while also demonstrating how such technology could be applied more widely.
“As this technology becomes more cost effective, it can be used to bring efficiencies to a complex supply chain. We now have the prospect of individually pre-planning surgical cases so that only the required implants and instruments specific to the patient are provided for the surgery at just the right time,” adds Dr Barker.
This is a major simplification of the way the majority of surgery is done when typically the requirements are only known at the time of the procedure, thus requiring large inventories of implants and instrumentation to be available for every case, adding time, cost and complexity. Combinations of such technologies can bring efficiencies to all elements of the surgical pathway and, as they become increasingly utilised, will enable surgeons ultimately to treat more patients.
We are continuing the tradition of pushing the boundaries of science, technology and clinical knowledge to achieve the very best for patients and keep people moving
“Through continuous innovation, for some surgeons the time to complete a typical knee replacement operation has been reduced to well under an hour. There is opportunity to bring that time down even further by increasing the use of pre-operative planning and linking it to automated tools in surgery, like surgical robots, to very accurately and quickly execute the complex bone cuts that were planned in advance,” says Dr Barker.
“These technologies bring more personalisation and automation to the treatment pathway, which may help to increase the predictability and reproducibility of the surgery, and the patient outcome.”
DePuy Synthes is also developing digital solutions to enable surgeons to support their patients more comprehensively. “We are developing technology and apps to enable surgeons to engage with their patients throughout their treatment so they are guided in preparing for an operation and then through a focused rehabilitation programme with tailored physiotherapy post-surgery,” says Dr Barker.
“This more personal approach could enable a patient to recover more quickly, leave the hospital sooner and achieve their best possible outcome, returning to their normal lives as soon as possible, while also reducing demand on hospital resources.
“Research is in our DNA and as we look to the longer-term horizon we are committed to innovating pioneering treatments, techniques and technologies that could enable earlier, less-invasive intervention and, in the future, even halt or reverse disease progression without ever requiring a traditional joint replacement.
“Our approach is to bring engineering expertise, surgical know-how and academic research together to drive the innovation process. Keeping people moving is our mission, but we also have a critical role to play in helping hospitals and surgeons meet the increasing demand in an environment of limited resources.
“We were involved at the start of modern joint surgery with Sir John Charnley, the British orthopaedic surgeon, who invented the gold standard cemented hip replacement in 1962. We are continuing the tradition of pushing the boundaries of science, technology and clinical knowledge to achieve the very best for patients and keep people moving.”