Doctors can now remove potentially debilitating and lethal blood clots in under an hour with technology that has just won the backing from five separate clinical trials.
The MR CLEAN study – Multicenter Randomised Clinical trial of Endovascular treatment for Acute ischemic stroke in the Netherlands – published in the New England Journal of Medicine, demonstrated brain tissue can be saved by directly removing the clots blocking major blood vessels to the brain which cause acute ischemic stroke.
The ability to target these clots with minimally invasive techniques means doctors can provide a safe and effective treatment in the time-critical moments after a patient is admitted with a suspected stroke.
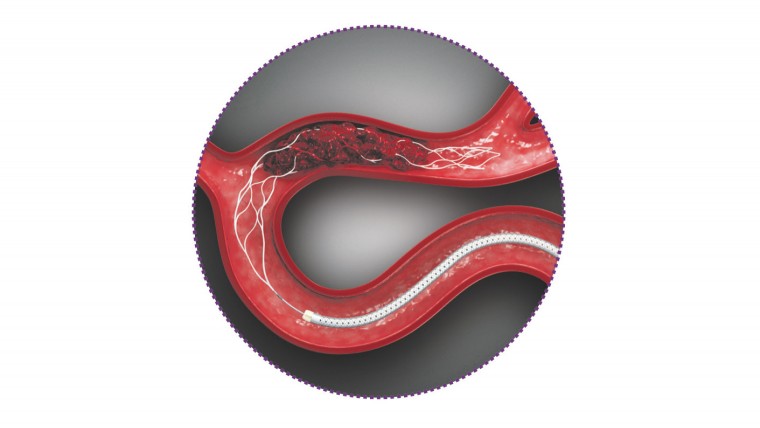
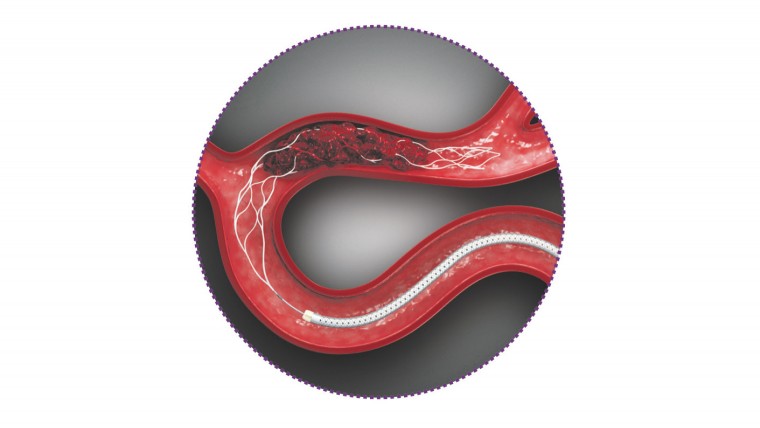
Trevo XP ProVue Retriever in Vivo
The results for patients are significant. While one in five who had standard tPA (tissue plasminogen activator) drug therapy were able to return to independent living, the figure rose to one in three with direct clot removal in the trial conducted with 500 patients in the Netherlands.
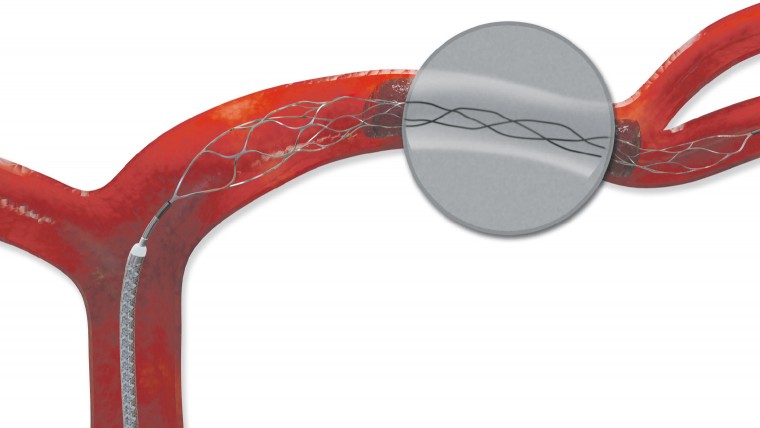
The treatment system uses a stent retriever – a cleverly designed wire mesh cage – delivered by a catheter that is inserted at the groin and directed up the femoral artery and through the blocked vessel where it expands to snare or capture the clot which is then drawn back out allowing normal blood supply to return.
Devices such as the Stryker Trevo® XP ProVue Retriever, which was approved by the US Food and Drug Administration in 2012, and the Covidien Solitaire™ FR Revascularisation Device are changing lives every day around the world.
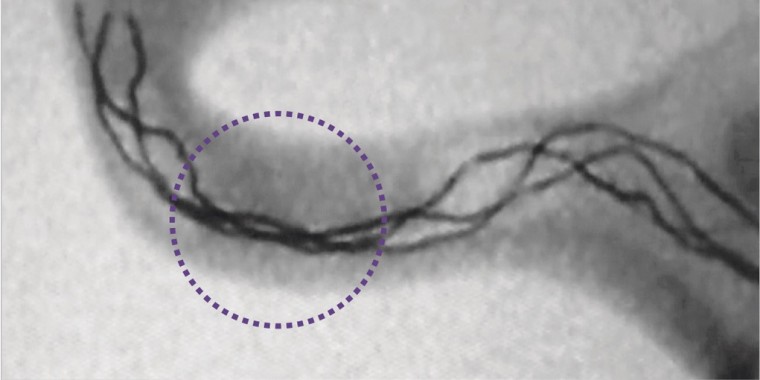
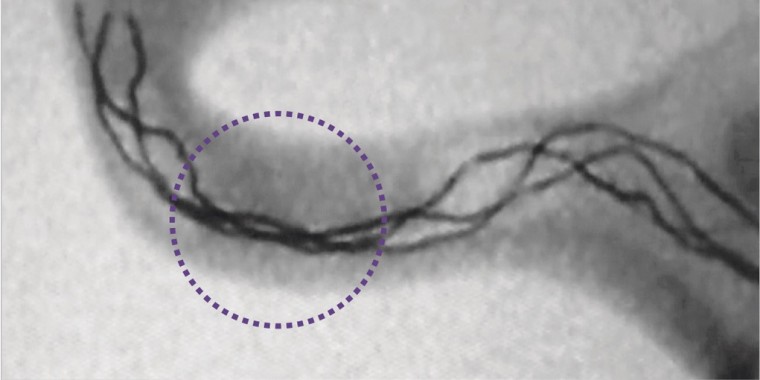
Trevo XP ProVue Retriever visible under fluoroscopy
In about one third to half of stroke patients, a clot lodges and occludes flow in one of the four large vessels feeding the brain with potentially devastating consequences.
People with smaller clots can be helped by tPA medication, delivered in the first three hours post stroke, which works to dissolve the clots. But it often does not help with big clots and no other treatments have been shown to work until now.
The success rate has been confirmed by the five trials, including MR CLEAN and ESCAPE in Canada, which included patients enrolled in Northern Ireland under the acute stroke care team and Dr Ian Rennie, consultant neuroradiologist at the Royal Victoria Hospital in the Belfast Trust Hospitals Group. This was the only hospital from the UK that participated in any of the five recently published trials.
“We have been carrying out this treatment for four to five years and have been doing increasing numbers recently,” says Dr Rennie. “We were part of the Canadian study which showed a huge positive benefit if we can get the patients for treatment quickly enough and well enough.
The ability to target clots with minimally invasive techniques means doctors can provide a safe and effective treatment in the time-critical moments after a patient is admitted with a suspected stroke
“By taking out the clots successfully, we can virtually halve their chances of dying and double their chances of a good outcome which is significant compared to the best medical treatment in terms of intravenous drugs.
“We have shifted the balance of probability of a good outcome from a big brain clot to 50-50 which, given the fact that without the treatment the patients may end up severely disabled or dead, is a major improvement.”
He says the devices have evolved to become so technically sophisticated that an interventional neuroradiologist could regularly remove clots within an hour, with the best treatment time of just under 20 minutes from the initial CT scan.
“Time is a critical factor with stroke,” says Dr Rennie, who believes the endovascular procedure system is destined to become commonplace in key hospitals, with other clinicians now achieving impressive and consistent clinical results.
“We had a patient in her early 40s who had a stroke. Because it is generally not thought about at that age, she came to us at six hours. She had a stroke scale that made us sufficiently concerned she would either die or be profoundly disabled and require nursing home care,” says Dr Rennie. “But she went home independently three or four days later. She and her family were delighted. We do get successes like that and the technology helps us achieve it.
“One of our early successes was a young patient, who fell asleep with the neck in an awkward position, on the way back from A-level exams and suffered a major blood clot at the back of the brain. It was a complex procedure with the earlier technology, but we were able to remove the clot. The patient was initially unwell, but improved greatly over time and we’re told the patient passed a driving test a year later.
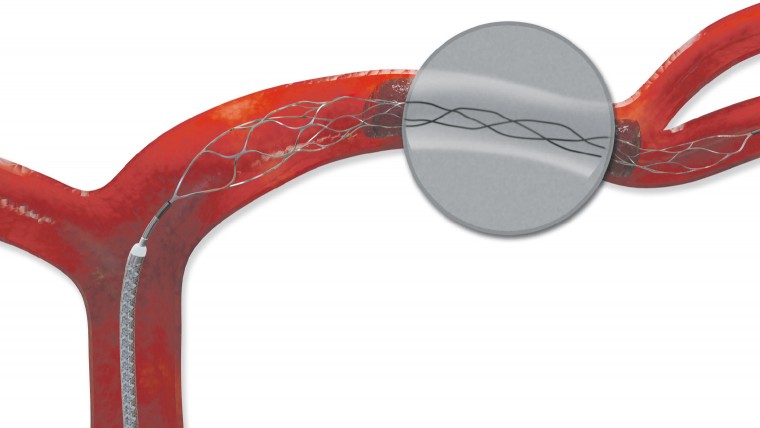
Trevo XP ProVue Retriever in Vivo
“That young patient is back to work, and will pay taxes and hopefully have a good life contributing to society. The operation at our end cost around £5,000 in devices, with the entire acute treatment costing about £10,000, whereas the patient could have ended up requiring long-term nursing home care at about £50,000 a year, every year.
“You can see how much that saves the NHS financially, but there is the ability to relieve the human suffering of a patient to endure the effects of a stroke for the rest of their life, so the costs are modest. The implications are significant.”
The system also synchronises with the ordered efficiency of an angiography room with stroke physicians or stroke neurologists where the staff and nurses work with slick calmness. “It is a bit like changing the wheels on an F1 car; once you’ve done the procedure a few times, it becomes very quick with everyone knowing their role,” says Dr Rennie. “We have now developed a very slick service.”
Patients can be receiving a local anaesthetic in preparation for the procedure just minutes after having their diagnosis confirmed by a CT scan. The ESCAPE trial target time was 90 minutes from CT to finish.
“It is a relatively simple procedure when carried out by an experienced team, and the design, technology and engineering has come on so much that we can quickly restore the blood supply to the brain and remove the clot efficiently,” says Dr Rennie, who with the local stroke team and colleagues treated 50 patients with the system during 2014 and has already reached this number five months into 2015.
“The potential is vast and I can see this becoming much more common around the UK,” he concludes.
The trial data has been welcomed around the world.